What Really Causes Death in Older Adults
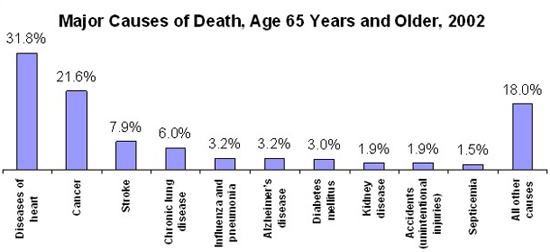
- “Old age” is not listed as a cause of death in the U.S. Instead, conditions such as heart disease, cancer, stroke, chronic lung disease, and dementia are common causes in people 65+.
- Many seniors experience multiple chronic conditions. Planning care around comfort and quality of life can reduce unnecessary hospital visits.